Reference for image https://www.bmj.com/content/364/bmj.l294 .
Physical therapy should be your first choice for shoulder pain, regardless of what’s causing it because it’s conservative, there are little to no side effects, and recent research suggests surgery is no better.
The shoulder is an incredible joint. As a ball-and-socket joint, it allows for an extremely wide range of motion and is the only type of joint that can rotate in a full circle around its axis. But as a result of its design, it’s vulnerable to injury. The rotator cuff can be pinched between the ball and a bone above the ball called the acromion. Also since the shoulder ball is much bigger than the socket, it makes the cartilage labrum around the socket also vulnerable to injury.
The issue is that the ball of the joint (the end of the upper arm bone, or humerus) is much larger than the socket (a structure called the glenoid fossa). Due to the major difference in size, the shoulder is considered an unstable joint, and the ball can slip out of the socket to cause pain and dysfunction. The good news is the rotator cuff helps actively hold the ball and socket together. One other feature of the shoulder that helps prevent dislocation is the labrum, which is a band of cartilage around the edge of the socket that adds depth and keeps the humerus in place. But despite this added protection, shoulder injuries are still quite common.
Two Diagnoses that Might (Yes, We Said “Might”) Cause Pain
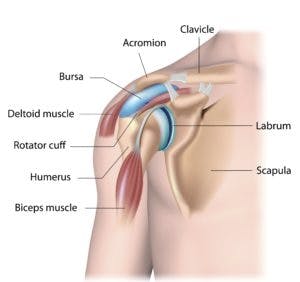
Shoulder impingement occurs when the rotator cuff tendons, primarily the supraspinatus tendon, is pinched between the humerus, subacromial bursa, and the acromion. See the above image to try to orient yourself. Imagine what could happen if the arm bone (the humerus) was raised overhead and pinched the rotator cuff and blue bursa that’s below the acromion bone. That’s what happens with shoulder impingement. It’s common but as indicated in the main image of this article at the top, recent research suggests that surgery isn’t better than conservative care.
While we agree that conservative care, especially provided by one of our professionally trained and licensed musculoskeletal experts, is the best thing to do first, we’ve also seen a number of patients that have had surgery and good outcomes as well. Bottom line, research often doesn’t adequately summarize all possible outcomes. Nevertheless, we agree with the research – you should first try conservative care before you have any surgical procedures.
Similar Research Suggests Conservative Care First for SLAP Lesions Too
A SLAP (superior labrum, anterior to posterior) tear is an injury to top of the labrum (or superior), from its front to back (anterior to posterior). SLAP tears can come about from a single incident, such as falling on an outstretched arm or shoulder, or from doing lots of overhead activities on a regular basis. Participation in overhead sports like baseball or tennis, or lifting heavy objects repeatedly can all increase the likelihood of experiencing a SLAP tear. In other cases, they result from the labrum gradually losing strength over time as a natural part of the aging process.
Typical symptoms of a SLAP tear include pain when moving the shoulder, a sensation of locking, popping, or catching, a decrease in shoulder strength and flexibility, and a feeling that the shoulder will suddenly “pop out.” If you’ve been experiencing these symptoms, a SLAP tear my be possible, and some medical professionals might recommend getting an MRI to confirm the diagnosis. While MRIs can be helpful, they should not be relied upon too heavily in these types of situations. Research has shown that the MRIs of many patients—particularly older individuals—with no shoulder pain will actually reveal the presence of a SLAP tear. For example, one study of 53 individuals between the ages of 45-60 concluded:
There is a high prevalence of superior labral tears diagnosed by MRI in the asymptomatic shoulders of middle-aged people. These findings suggest that superior labral tears noted by MRI may not be the cause of symptoms in this patient group with shoulder pain.
Regardless of whether a SLAP tear is responsible for your shoulder pain, physical therapy is the best first step to address it in nearly all situations. A physical therapist will work with you to identify the specific ways your condition is limiting you, and then create a personalized treatment program to address these impairments. Every program is different, but most will include the following:
- Flexibility exercises to stretch the shoulder capsule that surrounds the joint
- Strengthening exercises for the muscles that support your shoulder
- Manual therapy from the physical therapist to increase shoulder range of motion
- An analysis of your movement patterns and correction of any overhead faults
- Heat, ice, and/or electrical stimulation
Before you get an MRI of your shoulder in order to find out exactly what’s wrong, see a physical therapist. While specific diagnoses are helpful in some cases, they can also be distracting and take away from time that can be better spent getting treated and working your way back to full strength.
