Are you searching for plantar fasciitis treatment in Hanford that is long-lasting…more than the temporary relief you get from medication?
In this blog post, we will discuss the most recent clinical research for conservative and natural care for plantar fasciitis and shed light on the benefits of physical therapist-directed care.
We are Experts at Providing Effective Treatment for Plantar Heel Pain (pain on the bottom of your foot near your heel)

If you’re residing in Hanford, California, and seeking effective solutions for your plantar fasciitis, we can help. Our expert physical therapy team is here to provide you with treatment based on the current best science…plantar fasciitis treatment that can alleviate your pain and help you regain mobility.
Understanding Plantar Fasciitis and Its Impact – What is Plantar Fasciitis?
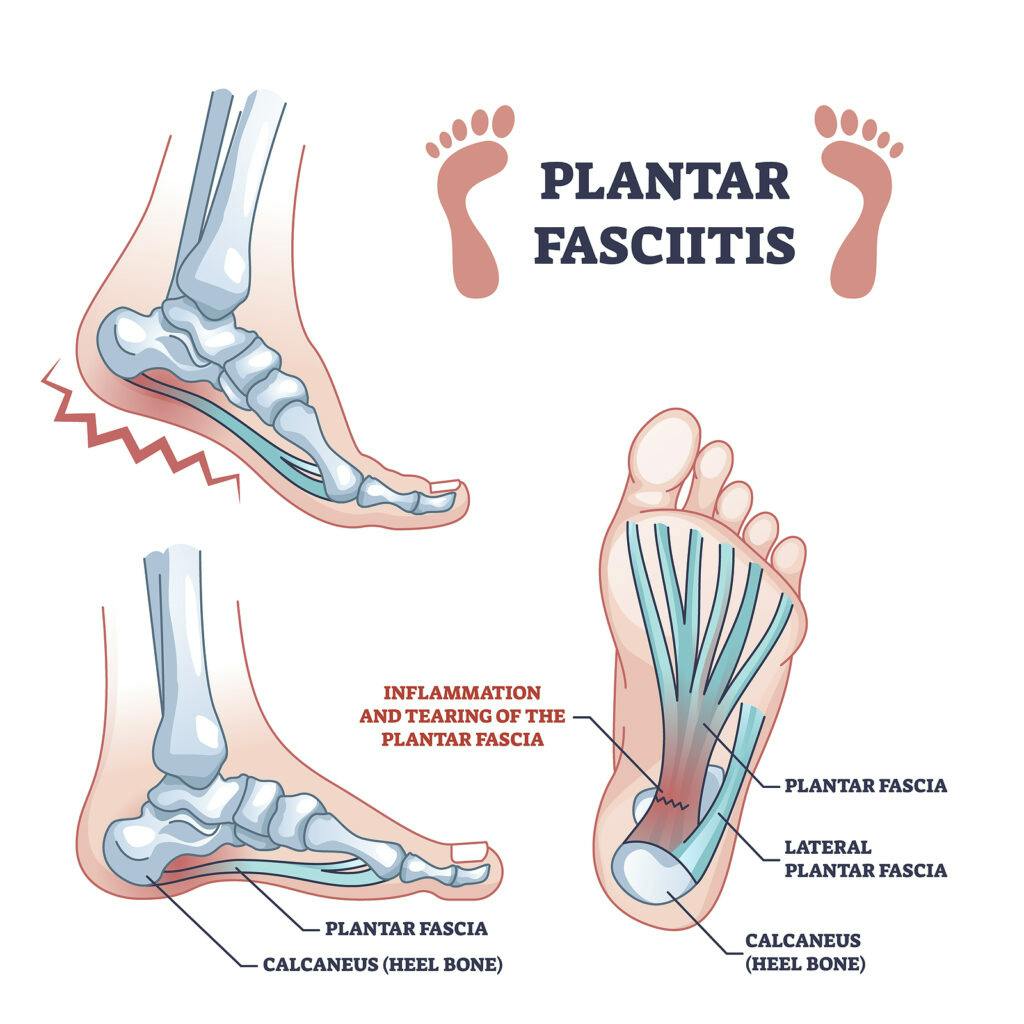
Plantar fasciitis is a common foot condition characterized by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of your foot.
This condition often leads to stabbing pain in the heel, which can worsen with prolonged standing, walking, or running.
It affects a significant portion of the population, including athletes and individuals with certain risk factors such as obesity or wearing improper footwear.
The Importance of Physical Therapist-Directed Care – Personalized Assessment and Treatment are Important
Seeing one of our physical therapist at our Hanford clinic for plantar fasciitis treatment is highly recommended, based on the most up-to-date clinical research. Consider this recent publication Level 1 research summary:
Management of plantar heel pain: a best practice guide informed by a systematic review, expert clinical reasoning and patient values
“The article is a guide of updated best practices for the evaluation and treatment of plantar heel pain (PHP), and is based on a systematic review, expert interviews, and a patient survey.
The review considered randomized controlled trials (RCTs) evaluating any intervention for people with PHP, with trials having a sample size greater than 38 being considered for proof of efficacy.
This study included 4351 participants from 51 eligible trials, with 9 RCTs being suitable to determine the proof of efficacy for 10 interventions.
The results showed good agreement between the systematic review findings and interviews of healthcare providers that regularly treat plantar fasciitis. The effectiveness of taping and plantar fascia stretching for reducing first-step pain was identified as an acceptable treatment in the short term.
The study suggests combining these interventions with education and footwear advice as the primary self-management approach.
Additional Treatments May Also be Helpful
For patients who do not show optimal improvement, the research recommends adding additional treatments such as focused shockwave for first-step pain in the short-term, medium-term, and long-term, and radial shockwave for first-step pain in the short and long term. The study also found good agreement to using custom foot orthoses for general pain in the short and medium term.
In conclusion, the best practice based on this mixed-methods study suggests that the core treatment for people with PHP should include taping, stretching, and individualized education. If patients do not optimally improve, they may be offered shockwave therapy, followed by custom orthoses 1“
Evidence-Based Treatment Techniques for Plantar Fasciitis Treatment Should Be What You are Looking For!

Our physical therapists are experts in musculoskeletal conditions and can provide a thorough assessment of your condition. They will evaluate your:
- Foot mechanics,
- Gait (walking patterns),
- Strength & flexibility, and
- Range of motion
Based on the evaluation results, we develop a personalized treatment plan tailored to your specific needs. By addressing the underlying causes of plantar fasciitis, physical therapists can target the root of the problem and provide effective solutions.
Your plantar fasciitis treatment plan may include some or all of the following:
- Manual Therapy: Skilled hands-on techniques, such as soft tissue mobilization and joint mobilization, can help reduce pain, improve tissue flexibility, and enhance overall foot function.
- Therapeutic Exercises: Physical therapists will guide you through a series of exercises to stretch and strengthen the plantar fascia and surrounding muscles. These exercises can promote healing, improve flexibility, and restore proper foot mechanics.
- Modalities: Additional treatments such as taping/strapping, ultrasound, electrical stimulation, or laser therapy may be used to complement the therapeutic plan and expedite the healing process.
The Benefits of Physical Therapist-Directed Care-Non-Invasive Approach

Physical therapist-directed treatments prioritize non-invasive (we don’t penetrate the skin with needles or drugs), natural approaches to alleviate plantar fasciitis symptoms. By emphasizing conservative interventions, we aim to avoid unnecessary surgeries and medications, reducing the risk of complications and side effects.
Long-Term Recovery and Prevention
One of the major advantages of our physical therapist-directed care is its focus on long-term recovery and prevention. Education on proper footwear, activity modification, and self-management strategies, physical therapists empower patients to take control of their condition and prevent future flare-ups.
It’s Important to Look at More Than Just the Foot & Ankle
Our physical therapists consider the entire kinetic chain when treating plantar fasciitis. They assess factors such as posture, lower limb alignment, and core stability to identify any contributing factors that may be exacerbating your symptoms.
By addressing these factors, physical therapists help you achieve optimal foot function and overall musculoskeletal health.
Call Us Today to Learn More & Get Started – Contact Us at (559) 582-1027
If you’re in the Hanford area and seeking effective plantar fasciitis treatment, look no further than physical therapist-directed care. By providing personalized assessment, evidence-based treatments, and a holistic approach to rehabilitation, physical therapists can help you overcome the challenges of plantar fasciitis and regain pain-free mobility. Don’t let plantar fasciitis hold you back—take the first step towards recovery by consulting a physical therapist today!